What is the
Heart Failure Collaboratory (HFC)?
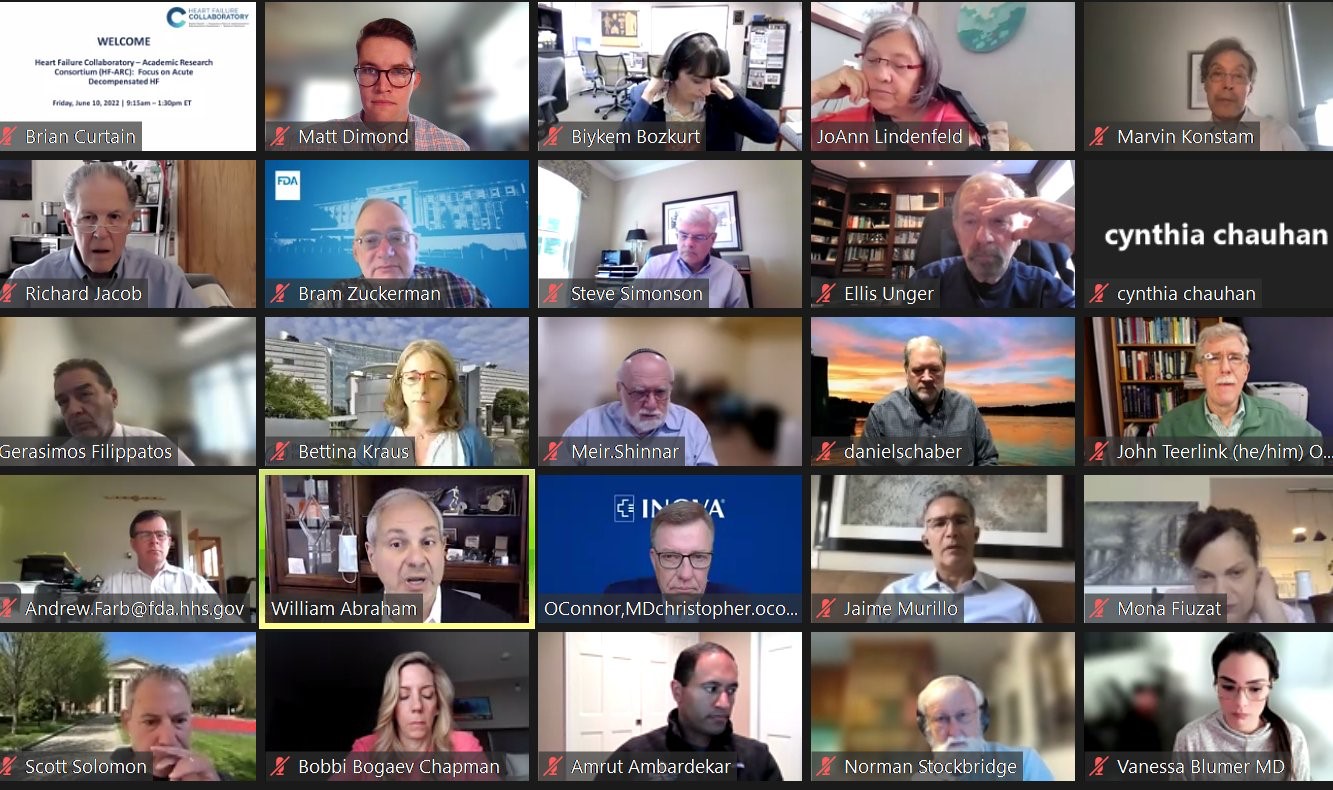
Efficiency of clinical trials and evidence generation in heart failure and foster development of therapies by creating a collaborative environment in which FDA, government agencies including NIH and CMS, and the heart failure community can interact to optimize innovation and advancement of new therapeutic products. HFC has established five working groups to tackle individual issues in clinical trials and fostering the development of effective heart failure therapies.
The Heart Failure Collaboratory is a public-private partnership with the FDA and the consortium to help foster the development of new products for heart failure.